Evidence based research to treat Hydrocephalus
Who We Are
Each year an estimated 10,000 people in the US and Canada will be diagnosed with hydrocephalus, a life-threatening and debilitating condition for which there is no cure.Many of these people are children. Left untreated, hydrocephalus can cause permanent brain damage, disability, and death. Most experts agree hydrocephalus occurs when the normal flow of cerebrospinal fluid (CSF), a natural fluid produced inside the brain, somehow gets restricted. This restriction results in increased pressure on a patient’s brain tissue.Our Mission
The mission of the Hydrocephalus Clinical Research Network (HCRN) is to dramatically improve the lives of kids suffering from hydrocephalus by conducting important and field-changing, multi-center clinical research.Our Vision
Our vision is that, in 5 to 10 years, doctors will use HCRN research-based evidence to improve the diagnosis, treatment and outcomes of hydrocephalus patients and that these patients will live longer, more trouble-free lives than they do at present. Over that same timeframe, we envision greater attention and financial resources directed toward hydrocephalus research and treatment.Our Research Initiatives
Reducing infections associated with shunt surgery.Understanding the epidemiology and outcomes of ETV.Creating a detailed registry of all hydrocephalus patients at participating institutions.Improving shunt placement using ultra-sound guidance.Management of hydrocephalus in premature children.Treatment of CSF shunt infection.
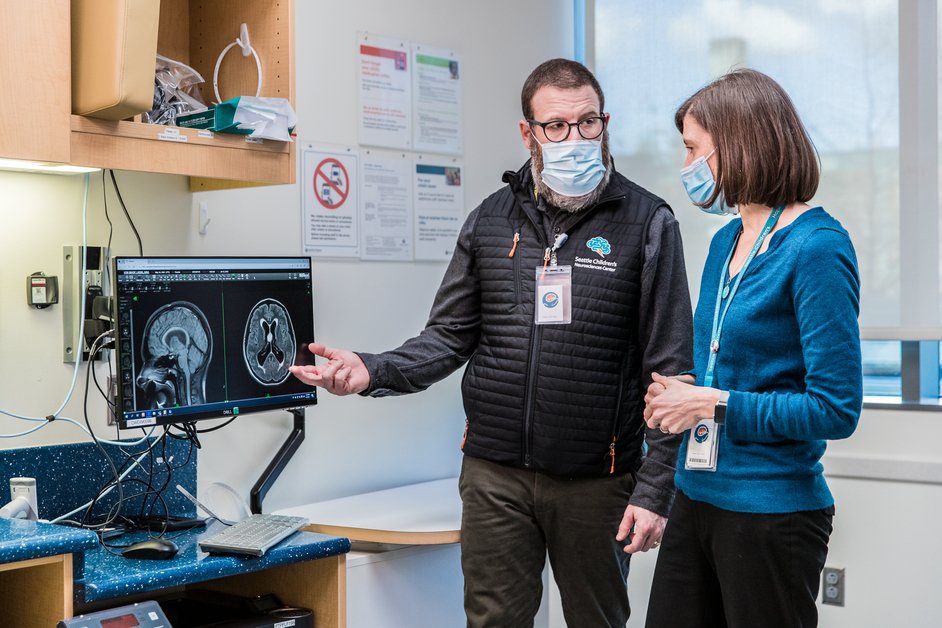
Our Team
Meet the team of Neurosurgeons, Statisticians, and Research Staff behind the HCRN